Background
The ILC team are equipment specialist therapists who support staff and the public across Devon. There has been increasing demand for support in managing people who have developed complex postures, and over the past three years Devon has been focusing on developing a Posture Care Pathway and upskilling therapy and care teams to manage people living with complex postural needs.
In 2023, the ILC invited Jo De Clercq of BV ComfortCare, world-renowned Belgian physiotherapist, to train Devon professionals on 24-hour Posture Care and Therapeutic Handling for people living with Dementia. Key to Jo’s approach is the understanding of and management of Paratonia, an involuntary increase in muscle tone present in 80 percent of people living with more progressed dementia. Paratonia is elicited in response to passive forces outside of the person’s control such as gravity and therapeutic handling. Paratonia is variable in terms of its magnitude and is affected by the speed and force being exerted on the person. With this in mind, Jo teaches that posture care is multifaceted and can be influenced not only by how someone is positioned, but also by how they are handled during care provision. Another important element to posture care emphasized in Jo’s Course are the sensory influences from the external environment which can elicit the flight, fight or freeze response if the person becomes over stimulated.
In April 2024, the ILC Physiotherapist, was granted funding to attend a day’s shadowing opportunity at De Wingerd residential care home in Belgium. De Wingerd was set up in 2008 with a vision to provide normalised, small-scale living for people living with dementia. During the shadowing experience the ILC physiotherapist spent time with Jo De Clercq, & Karen Claes Senior Physiotherapist, to see how they manage posture care at De Wingerd. Jo is responsible for ComfortCare & Care Innovation for Woonzorgnet Dijleland, to which De Wingerd belongs. This article shares the key learning points from the shadowing experience and how it relates to the work being done in Devon.
Therapeutic Handling: The Turn Only Once Principle:
The day at De Wingerd began with discussing the barriers to providing Posture Care within the care home setting. Jo talked about how introducing postural care can be perceived to be increasing the care burden on staff in the short term. When introducing posture care at De Wingerd, Jo explained that he started with using the Turn Only Once Principle (TOO), a technique designed to deliver personal care whilst minimising moving and handling and distress to the person receiving care. If the TOO principle is delivered correctly, this reduces the paratonia response as much as possible and makes care provision more time efficient. Jo and his team trained the carers at De Wingerd to deliver TOO and they quickly realised that it was quicker and easier to provide care in this way, often enabling single handed/1-1 care provision. In addition, carers also had time to put bed positioning in place as part of the care provision which also had a significant beneficial impact on the person’s tone and posture over time.
During the visit to De Wingerd, it was really useful to experience the TOO principle being carried out with a resident. The technique was quick and easy to perform, only required one carer, and the resident seemed relaxed throughout. The method involves using specialist equipment which significantly reduces the need to turn, move or handle the person during care provision. The equipment used included:
- a one-piece incontinence pad with belt closure
- one pack of 8 pre-moistened soft wash gloves with lotion, as alternative to water, soap & towels
- adapted clothing
In further discussion with Jo, he explained that the TOO principle is not only a powerful way to engage carers with posture care but also is key to the ongoing success of 24 posture care at De Wingerd. He explained that if the resident starts their day with personal care that elicits paratonia, the person’s tone is already affected and is more likely to increase over the course of the day. The cumulative effect of this over weeks and months, is a significant factor in whether someone goes on to develop contractures. Therefore, without addressing this therapeutic handling aspect of Postural Care, the impact of providing structural posture support in lying and sitting is limited. The ILC are looking to develop a way to adapt the TOO principle to make it affordable and practical to implement in Devon. Other areas in the country such as Wales are also looking into piloting the TOO principle so watch this space.
Providing structural Posture support in lying and sitting:
The MC5 Mobility Class 5 scale (see image below), from Locomotion, is used at De Wingerd to help plan a person’s posture care. Following on from Jo’s course in 2023, this scale is now being used in some care homes within Devon. The ILC are incorporating this into a Posture Care matrix to guide clinicians and multi-disciplinary teams in the management of someone’s posture & pressure care needs over a 24-hour period at different stages of disability.
Jo and Karen explained that at De Wingerd, structural posture support in lying is not usually implemented in the early stages of someone’s disease. However, postural support in standing is considered at these early stages by careful selection of walking aids and transfer equipment. Bed positioning is usually only introduced in the D and E phases, and sometimes the C phase of the MC5. Jo and Karen explained that it is not uncommon that a resident can fluctuate through several stages of the MC5 scale in one day which is usually an indicator that their care needs to be adapted in order to stabilise their presentation. It can also mean that posture care in bed is sometimes phased into someone’s care plan overtime and built up as required.
At De Wingerd they favour using modular bed positioning systems to stabilize & sensory inform the person. These systems enable the person to be held in a stable and comfortable position whilst immersing & enveloping them. Jo and Karen explained that the immersive aspect, mainly provided by the overlay creating a cocooned/cradled position, is really important with dementia. In Devon due to the risks of using modular systems incorrectly which could impact the person’s skin integrity, we have been using individual posture support cushions instead. However, as care provider knowledge and expertise grow in this area we hope we will be able to move towards using modular bed positioning systems more in Devon. Photos below show images of modular bed positioning systems being used in practice.

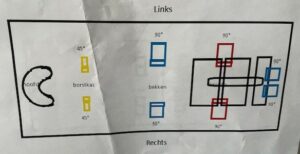
At De Wingerd, providing carers with training and education on how to put bed positioning systems in place, is very important. All new care staff receive training in implementing bed positioning and an important part of this training is getting the carers to feel it themselves. This is a powerful way to help them understand how it feels for the person and how comfortable and reassuring it is. Simple diagrammatic 1-page plans are used for carers to follow and therapists monitor whether systems are being put in place accurately (see photo below). As in Devon, it is recognised at De Wingerd that there is an ongoing need for therapists to continuously monitor this.
In terms posture support in sitting, immersive and enveloping seat bases are promoted at all stages to promote sensory feedback & stability. At the E phase of MC5, fully immersive & enveloping seating helps the resident feel cocooned/cradled and fully relax in sitting (see photos below). The chairs can also be tilted in space so gravity can contribute by sensory informing & stabilising the person. However, due to lower incidence of destructive posture change there is less need for the chairs to be fully adaptable. Jo and Karen also discussed the importance of not sitting the person out for too long especially in the E phase of MC5, and timing sitting out with when family and friends visit. In Devon we are constantly reviewing the types of seating we are recommending to clients and care providers. Seeing what seating is being used at De Wingerd was a useful insight and will help guide future equipment choice.


Other factors to consider in Posture Care and the importance of involving the person’s family:
Jo and Karen explained that throughout the day, other factors can also influence someone’s tone and posture. Subtle environmental and emotional factors such as a loud television, upsetting images on the news or sitting in a room with lots of people can lead to overstimulation and elicit the fight, freeze &/or flight response (FFF) which in turn can increase muscle tone. Increased muscle tone elicited in this way is a non-verbal signal/behaviour from the person to ‘say’ that they are sensory overstimulated due to secondary environmental/sensory input. This in turn will affect their ability to feel their own body via their primary sensory mechanisms (touch, proprioception and vestibular) and the person will start to become over whelmed and switch into FFF. With this in mind creating an environment which better suited to the sensory needs of people living with dementia is an important part of their postural management.
At De Wingerd, the care home is organised into smaller houses with no more than 8 residents in each, avoiding the need for people to sit in large groups. The television in communal areas is put on low and is mostly showing calming images/photographs with light classical music in the background. The news is avoided although residents can watch the news in their own room if they wish. The set up at De Wingerd is also geared towards ensuring the person feels part of a meaningful social group and that friends and family visit regularly. In fact, the latter is a prerequisite to the person becoming a resident at De Wingerd. Another important part of the resident’s social engagement is for them to join in group activities or events going on in the home. At De Wingerd they run daily activities and groups for residents and families which the ILC Physiotherapist also had the opportunity to observe during the visit. Staff ensure that residents only join these activities which are appropriate for their cognitive level and sensory processing capacity to avoid over stimulation.
Staff and family are educated on the factors above and taught how to recognise if someone is becoming over stimulated or if their emotional/social needs are not being met. Changes in; behaviour, cognition, posture, body language and or muscle tone are all behavioural signals to look out for. At De Wingerd the resident to staff ratio is relatively high (8/1), however, family and friends also play a part in this monitoring process. This facilitates close monitoring of the residents over a 24-hour period allowing the appropriate intervention to be carried out. If residents do become over stimulated from the environment there are several therapies offered at De Wingerd that help calm the person. The therapies are aimed at calming the person by lowering the amount of secondary environmental/spatial sensory input & increasing primary physical sensory input. This primary input includes tactile, proprioceptive and vestibular information to help sensory inform the person. The therapies include floating towelled bathing (below right), music therapy, water beds (below left) & mechanical rocking chairs. Sometimes the person may also just benefit from being taken back to their room for a sensory rest to help calm them down.

Families are also educated about the different stages of dementia using the MC5 mobility scale. The pictures of the MC5 provide an easy way to explain how dementia progresses and how this will impact on their relative’s care needs. This helps prepare families for the inevitability that their relative will be become less able over time and will need more time spent in their own room and less time sat out in their chair. Towards the end stages of a person’s life at De Wingerd sitting out in a chair is usually only reserved for when family visit and sometimes not at all. It is important that the persons family understand that sitting someone out can do more harm than good if they can no longer tolerate it without it having adverse effects. Fatigue management and tolerance of activities such as sitting out in a chair is an important part of posture care and care planning.
Conclusion:
The unique set up and high level of expertise in Posture Care at De Wingerd lends itself to being able to deliver such a successful and integrated model of posture care. It is clear to see that De Wingerd is delivering gold standard posture care with people living with dementia. Devon is already adopting some aspects of their care model, however, the learning from the shadowing experience highlighted the need to focus more emphasis on therapeutic handling and other environmental factors as part of our posture care pathway. Key to the successful implementation, and a cornerstone of posture care at De Wingerd, was the introduction of the TOO principle. The next logical step would be to see if this can be adopted within Devon using an adapted approach. If carried out correctly, TOO is aimed at being more time efficient and involving less carers. The benefits of this approach are widespread, not only in terms of posture care and reducing the financial cost of care but also by reducing the physical & mental workload on care providers.